Sun Exposure Triggers Your Skin to Make More Melanin, Leading to More, and Darker, Pigmentation

The Essential Info
The red/dark marks that are left behind after acne lesions heal are known as hyperpigmentation, and are a common problem, particularly in non-Caucasian people.
Sun exposure does not cause hyperpigmentation, but the sun’s rays can make existing hyperpigmentation worse by increasing skin pigment (melanin) production, making the marks more noticeable and longer-lasting.
If you are prone to hyperpigmentation, try to keep these marks out of the sun and/or wear a broad-spectrum sunscreen with an SPF of 15 or higher to prevent them from getting worse or lasting longer than they should.
Keep Vitamin D in Mind: Any time I caution people to limit sun exposure, the next thought I have is, “Well, what about vitamin D?” We get vitamin D primarily through exposing our skin to the sun, and the darker the skin, the more time that is required in the sun to achieve adequate levels of vitamin D. Maintaining a healthy level of vitamin D may be important when it comes to acne as well, so, if you’re limiting your sun exposure, get your vitamin D levels checked, and supplement if your doctor recommends it.

The Science

Hyperpigmentation refers to any disorder that causes a darkening of the skin, usually in patches or spots, including the darkening of the skin that happens after an acne lesion heals.
Hyperpigmentation occurs due to extra melanin production, and is much more common in people with non-Caucasian skin, who tend to genetically produce more melanin.1 One scientific article that reviewed studies performed in women with acne concluded that hyperpigmentation occurs in 65% of Black women, 48% of Hispanic women, 25% of White women, 18% of Asian women, and 10% of Indian women. Patients with darker skin who have hyperpigmentation often report that the hyperpigmentation is actually more distressing than the acne itself.2
Melanin is a natural pigment that gives the skin its color and also protects skin from the sun. It is made by skin cells called melanocytes, which sit at the bottom of the outer layer of skin.1 Since sun exposure creates extra melanin, it can make hyperpigmentation worse.
First, let’s look at how hyperpigmentation occurs, and then we will explore how the sun makes it worse and why it’s important to protect your skin from the sun if you are prone to hyperpigmentation.
How hyperpigmentation occurs
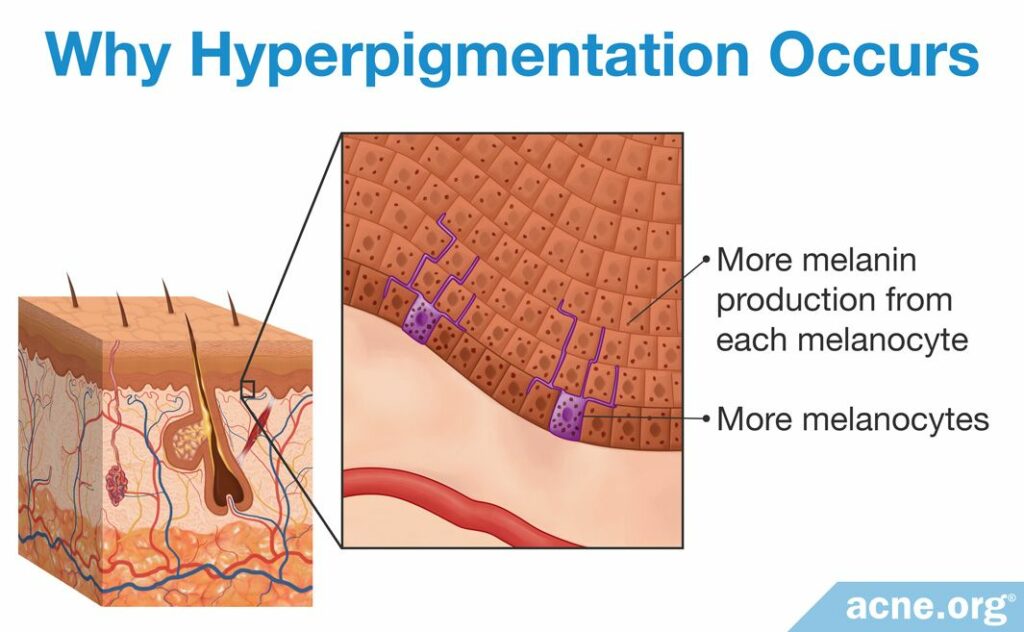
Usually, melanocytes and the melanin they make are equally distributed throughout the skin, leading to an even skin tone. In hyperpigmentation conditions, like hyperpigmentation caused by acne lesions, the skin makes more melanin in one location, in one of two ways:
- By increasing the number of melanin-producing melanocytes
- By increasing the amount of melanin the melanocytes make
The extra pigment then makes that bit of skin darker than the surrounding area, leading to a noticeable patch or splotch.1,3
In hyperpigmentation that is left behind after acne lesions heal, the spots can be red, brown, or even gray-blue colored, depending on the color of the skin and how deep into the skin the hyperpigmentation goes. These spots can stick around for several months to several years, if not longer, but are not scars and do ultimately fade with time.5,6
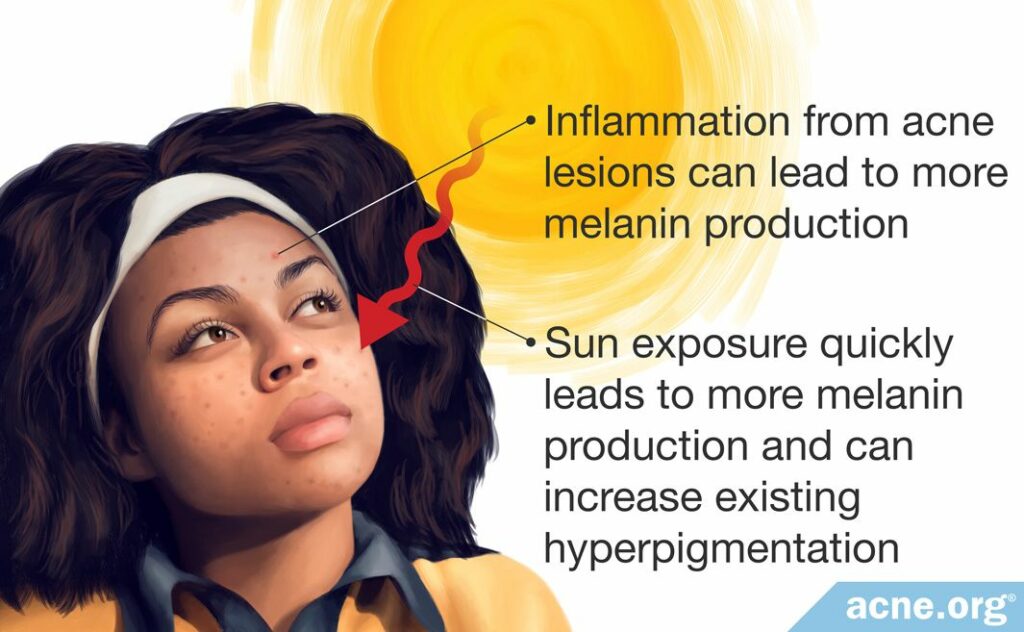
Why hyperpigmentation occurs in acne
In acne, the extra melanin results from inflammation at the site of acne lesions. For this reason, it is considered a specific type of hyperpigmentation called post-inflammatory hyperpigmentation.4,5 Regardless of how hyperpigmentation occurs, it is usually treated the same, and keeping any type of hyperpigmentation out of the sun is important.
How the Sun Makes Hyperpigmentation Worse
Melanin is the skin’s way of protecting itself from the sun, and the skin will quickly produce more melanin any time it is exposed to the sun’s rays. This is the simple reason why sun exposure makes acne hyperpigmentation worse. The more sun exposure, the more melanin the skin produces to protect itself.4
Melanin has a remarkable ability to absorb UV rays and protect your skin from the sun by preventing the sun’s rays from damaging DNA and other parts of skin cells. You can see this in action if you spend time in the sun and get a suntan. That extra color comes from extra melanin.
The problem is, with hyperpigmentation, extra melanin is the last thing you need. Dark patches on your skin can become darker, and they can also last longer.
In addition, research also shows that UV rays from the sun stimulate inflammation, which, at least in theory, might further increase hyperpigmentation.7
How to Treat Acne Hyperpigmentation
Because hyperpigmentation gets worse in the sun, one way to make sure that it fades as quickly as possible is to avoid direct sun exposure, and keep any skin with acne hyperpigmentation out of the sun through protective clothing or hats and/or sunscreen whenever the skin is directly exposed to the sun.5 Dermatologists recommend broad-spectrum sunscreens with SPF values of 15 or higher.6
Importantly, when it comes to hyperpigmentation, darker-skinned people need to protect their skin from the sun just as much as lighter-skinned people. While dark skin is less likely to burn in the sun, it is actually more likely to develop hyperpigmentation, so protecting the skin with clothing, sunscreen, or by staying in the shade is key.8

Once you have your skin protected from the sun, there are topical treatments that you can apply to your skin that can help quicken the fading of hyperpigmentation, including:6,9
- Hydroquinone
- Retinoids
- Kojic acid
- Azelaic acid
- Glycolic acid
Some of these are skin-bleaching agents that prevent melanin production, while others encourage cells to turn over faster so you shed the ones with the extra melanin more quickly.
For severe hyperpigmentation, chemical peels and laser treatment may also be helpful.10,11
The Bottom Line
If you tend to have red or dark marks that linger after acne lesions heal, firstly and most importantly, you want to clear your acne to prevent future battles with this kind of lingering hyperpigmentation. However, to ensure that these marks fade as quickly as possible, it is also important to keep hyperpigmented skin out of the sun or wear broad-spectrum sunscreen to help the marks fade more quickly.
References
- Stulberg, D. L., Clark, N. & Tovey, D. Common hyperpigmentation disorders in adults: Part I. Diagnostic approach, café au lait macules, diffuse hyperpigmentation, sun exposure, and phototoxic reactions. Am Fam Phys 68, 1955 – 60 (2003). https://www.ncbi.nlm.nih.gov/pubmed/14655804
- Callender, V. D., Baldwin, H., Cook-Bolden, F. E., Alexis, A. F., Stein Gold, L. & Guenin, E. Effects of topical retinoids on acne and post-inflammatory hyperpigmentation in patients with skin of color: A clinical review and implications for practice. Am J Clin Dermatol 23, 69-81 (2022). https://pubmed.ncbi.nlm.nih.gov/34751927/
- Stulberg, D. L., Clark, N. & Tovey, D. Common hyperpigmentation disorders in adults: Part II. Melanoma, seborrheic keratoses, acanthosis nigricans, melasma, diabetic dermopathy, tinea versicolor, and post-inflammatory hyperpigmentation. Am Fam Phys 68, 1963 – 8 (2003). https://www.ncbi.nlm.nih.gov/pubmed/14655805
- Potrądzikowa, H., Przegląd, K., Kishan, H., Yadalla, K. & Aradhya, S. Post acne hyperpigmentation: A brief review. Our Dermatol Online 2, 230 – 231 (2011). https://www.researchgate.net/publication/236335341_Post_Acne_Hyperpigmentation_A_Brief_Review
- Chandra, M., Levitt, J. & Pensabene, C. A. Hydroquinone therapy for post-inflammatory hyperpigmentation secondary to acne: not just prescribable by dermatologists. Acta Derm Venereol 92, 232 – 5 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22002814
- Trivedi, M. K., Yang, F. C. & Cho, B. K. A review of laser and light therapy in melasma. Int J Womens Dermatol 3, 11 – 20 (2017). https://www.ncbi.nlm.nih.gov/pubmed/28492049
- Gabros, S., Nessel ,T. A. & Zito, PM. Sunscreens And Photoprotection. [Updated 2020 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537164/
- Davis, E. C. & Callender, V. D. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol 3, 20-31 (2010). https://pubmed.ncbi.nlm.nih.gov/20725554/
- Lynde, C. B., Kraft, J. N. & Lynde, C. W. Topical treatments for melasma and post-inflammatory hyperpigmentation. Skin Therapy Lett 11, 1 – 6 (2006). https://www.ncbi.nlm.nih.gov/pubmed/17075653
- Zawar, V. P., Agarwal, M. & Vasudevan, B. Treatment of postinflammatory pigmentation due to acne with Q-switched neodymium-doped yttrium aluminum garnet In 78 Indian cases. J Cutan Aesthet Surg 8, 222-226 (2015). https://pubmed.ncbi.nlm.nih.gov/26865787/
- Nautiyal, A. & Wairkar, S. Management of hyperpigmentation: Current treatments and emerging therapies. Pigment Cell Melanoma Res. 34, 1000-1014 (2021). https://pubmed.ncbi.nlm.nih.gov/33998768/
 Acne.org Products
Acne.org Products