The Biggest Difference Is that Females Can Elect to Use Oral Contraceptives and/or Oral Anti-androgens

The Essential Info
Males:
- Due to higher levels of male hormones, adolescent boys and young men have thicker skin that produces more skin oil. On the whole, this leads to more severe acne when compared with their female counterparts, which means more aggressive treatment is sometimes required.
- Since males develop facial hair, it can be harder to apply topical medications, so it is best for males who are applying topical medications to shave every day so that those medications can be evenly applied to the skin.
Females:
- Hormonal treatments like oral contraceptives and anti-androgens are almost never prescribed to males, but can be effective in females.
- There is some initial evidence showing that some topical acne medications might work slightly better in females compared to males.

The Science
- Male Hormones
- Hormonal Treatments
- Facial Hair
- Some Acne Treatments May Work Better in Females
- Conclusion
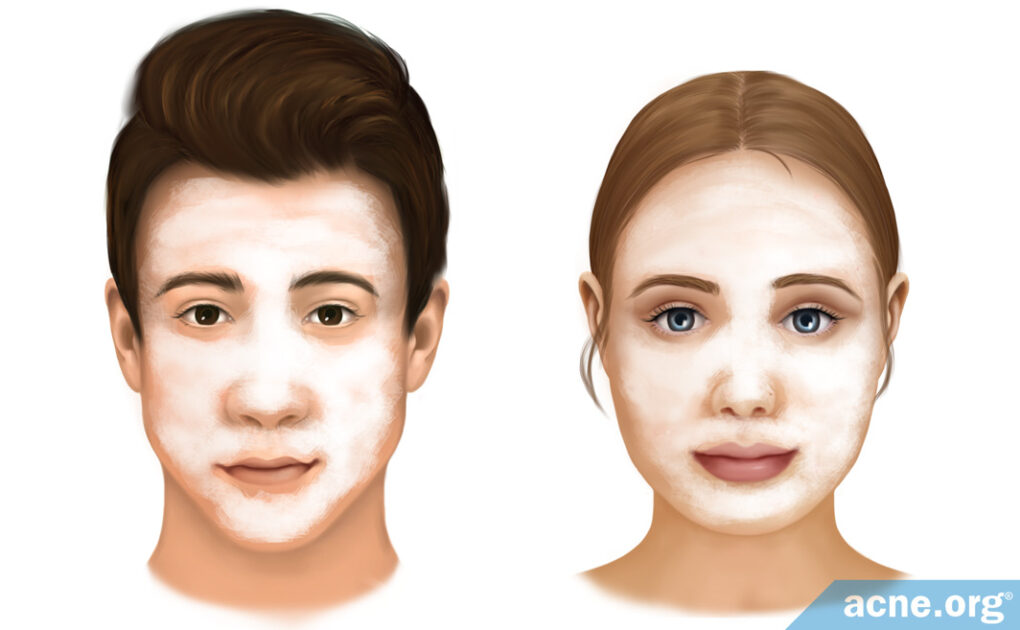
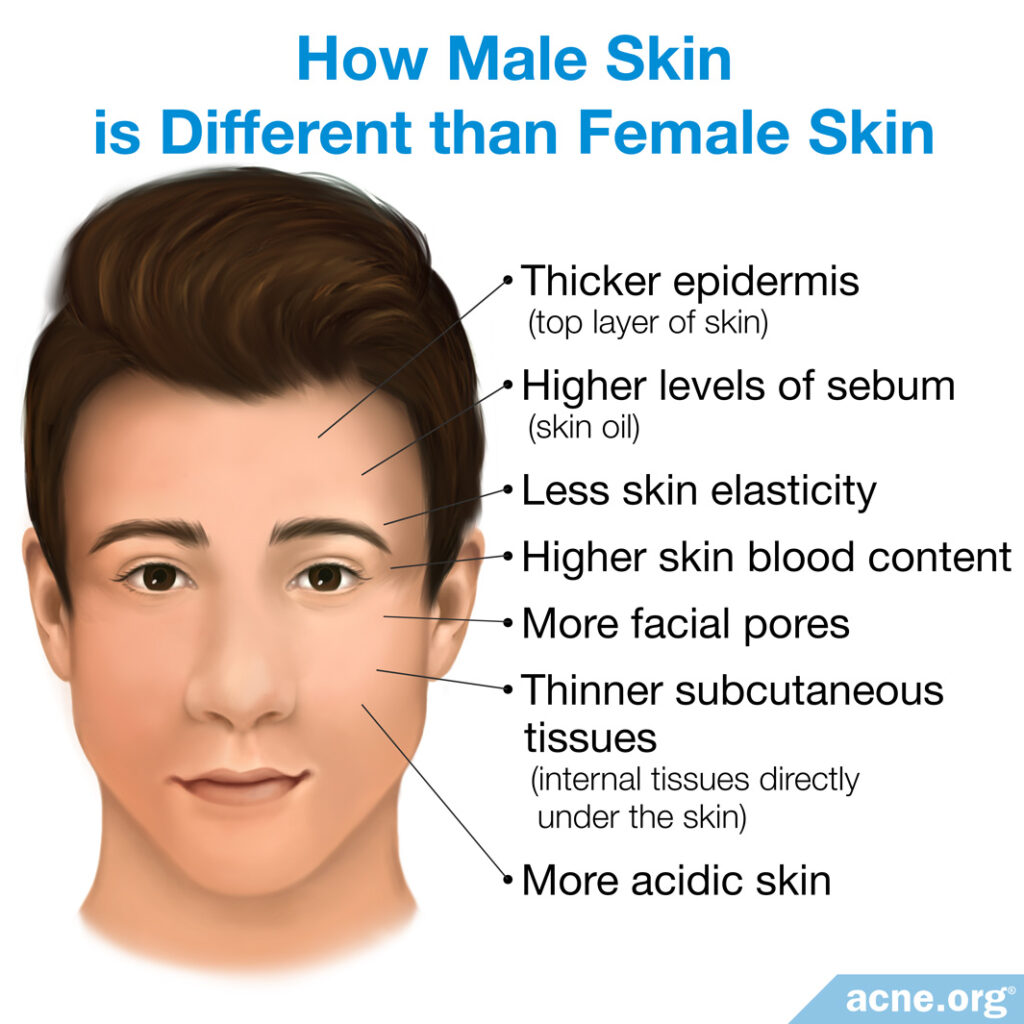
Due to higher levels of male hormones (androgens), the skin of males is different from that of females.
Males have:
- A thicker epidermis (top layer of skin)
- Higher levels of sebum (skin oil)
- Less skin elasticity
- Higher skin blood content
- More facial pores
- Thinner subcutaneous tissues (the internal tissues directly under the skin)
- More acidic skin1
Female skin is the opposite:
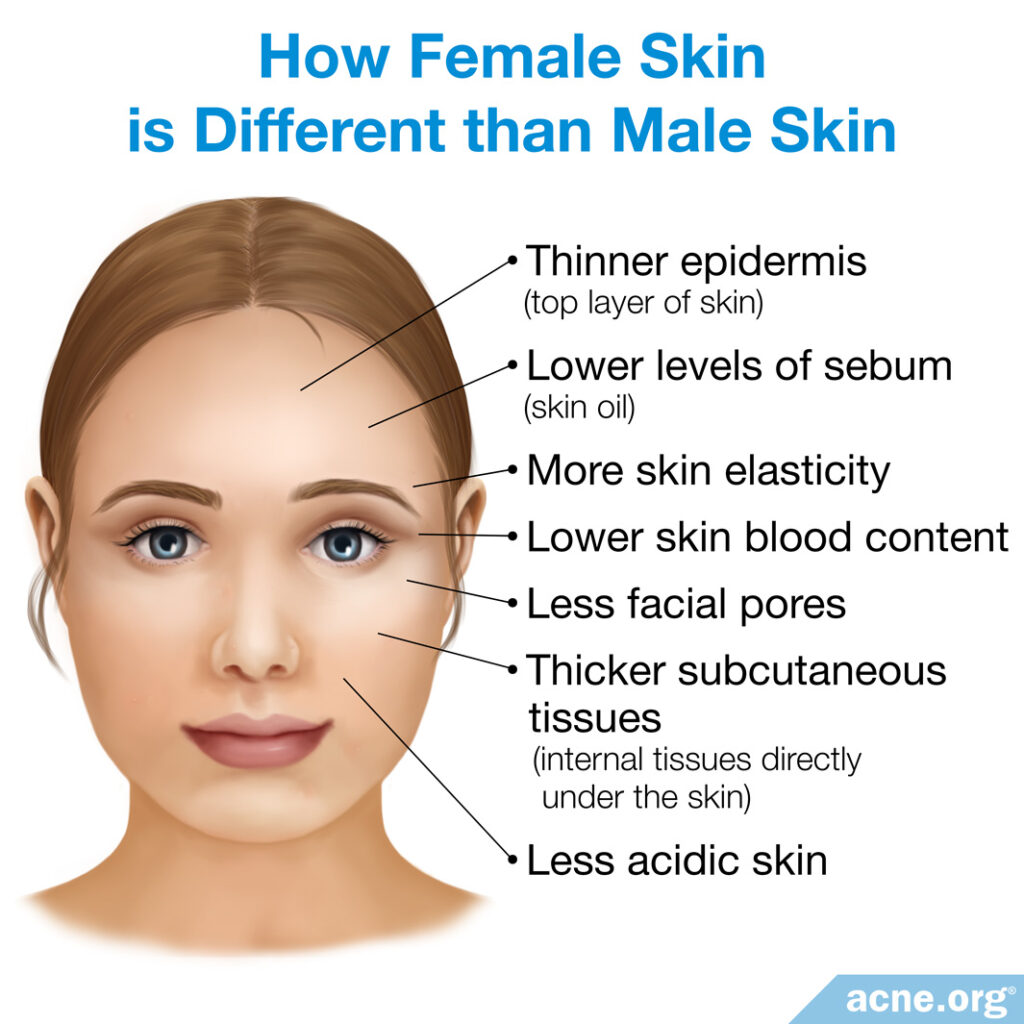
Since males tend to have higher levels of sebum (skin oil), and higher levels of sebum tend to go hand in hand with more acne, this is an important reason why males tend to develop more acne than females. Females on the other hand have less acidic skin, which may provide a more ideal breeding ground for acne bacteria.
A 2006 study backs up these points.2
Expand to read details of study
A 2006 study in the Journal of Dermatological Science found that:
- Higher amounts of sebum, which generally occurs in males, appears to increase the likelihood of developing acne.
- Skin that is less acidic appears to encourage the growth of a type of bacteria, C. acnes, which increases the chances of developing inflammatory acne.2 This is an interesting observation because even though females have less acidic skin, acne actually affects males more often than females. This would indicate that less acidic skin, which occurs in females, has less impact than sebum levels on the development of acne.
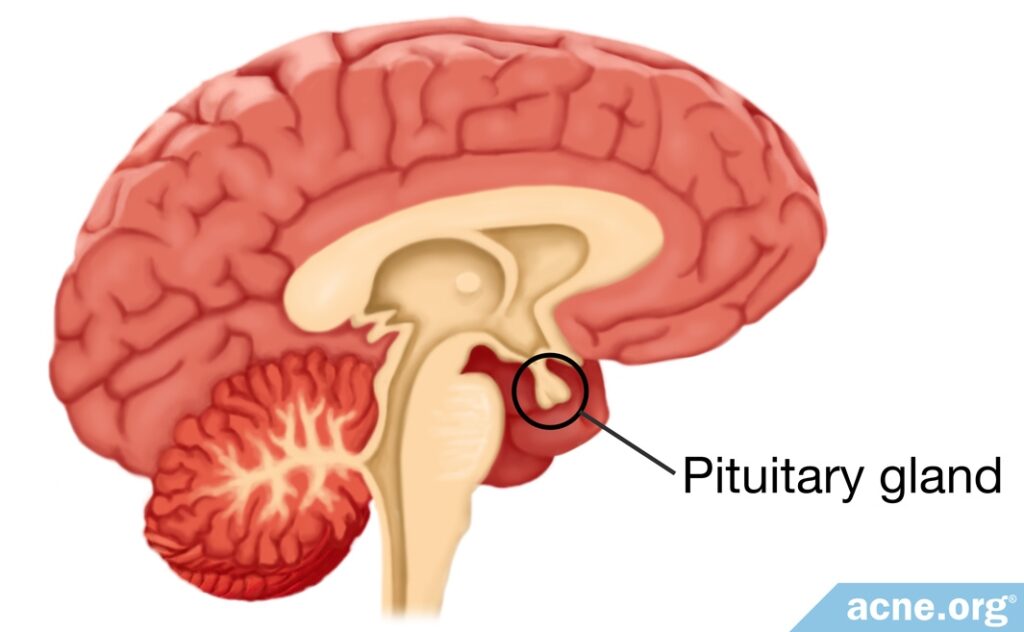
Male Hormones Play a Major Role in the Development of Acne
When it comes to acne, the role of androgen hormones (male hormones present in both males and females) should not be underestimated. These hormones are a necessary condition for acne to develop, and the fact that males end up producing more male hormones like testosterone explains why they are more likely to develop acne as well as to have more severe acne compared to females.
Expand for details of how male hormones influence acne
Humans do not develop acne unless they have testosterone in their blood. A 2005 study in Experimental Dermatology drives this point home:

According to the authors of the study, “Several clinical observations point to a major role of androgens in the [development] of acne…[A]cne begins to develop [at the onset of puberty] when the adrenal gland starts to produce large quantities of…a precursor for testosterone.”3
These observations explain why acne tends to develop during puberty in both males and females, when production of testosterone increases, and why males, who end up producing much higher levels of testosterone, are more prone both to acne in general and to more severe acne.
In addition to the normal increase in androgens that comes with puberty and the differences in androgen levels between males and females, sometimes people of either gender can have abnormally high levels of androgens. Excessively high androgen levels are associated with:
- Increased secretion of sebum (skin oil)
- The development of severe acne in both males and females3
Generally speaking, it appears that both males and females with severe, persistent acne typically have higher blood levels of androgens than those without acne. They also have higher levels of androgens compared with people who have less severe acne.4,5
Hormonal Treatments – Usually For Females Only
When acne is caused by abnormally high androgen production, estrogens and anti-androgens can help counteract the effects of these androgens. Doctors prescribe these two options far more often for female patients, since they can cause feminization in males, such as the growth of breast tissue.
Estrogens are female sex hormones. They work by reducing both the size of the glands that produce sebum and the amount of sebum that these glands produce.4 Estrogens are prescribed to only females in the form of oral contraceptives (birth control pills), and are effective in reducing androgen levels. For mild-to-moderate acne, contraceptives that contain mostly estrogen usually reduce acne, on average, by 60%. For more severe acne, or if there is no improvement with contraceptives containing mostly estrogen, switching to contraceptives that contain a type of hormone called progestogen may improve response. For acne that doesn’t improve with contraceptives alone, adding an anti-androgen medication is usually effective.6

Anti-androgens, such as spironolactone, are medications that block the effects of androgens, thus reducing the production of sebum. They are usually prescribed only to females, but their power to reduce acne has been shown in both females and males in clinical trials.3,7
According to one study, males and females with therapeutically resistant, severe, persistent acne, known as “cystic acne,” typically have abnormally high androgen levels and benefit from estrogen and/or anti-androgen treatment.8
Expand to read details of study

In a 1983 study in The New England Journal of Medicine, males with cystic acne were given anti-androgens and females with cystic acne were given oral contraceptives and/or additional anti-androgens. The authors noted, “Of the patients treated for six months, 97 percent of the women and 81 percent of the men had resolution or marked improvement in their acne.”8
Topical Hormonal Treatment: Can It Be Effective and Safe for Both Males and Females?
Recently, the U.S. Food and Drug Administration (FDA) approved a new topical anti-androgen called clascoterone for treating acne in both males and females aged 12 years and up. Researchers believe that clascoterone works by blocking androgen receptors in the glands that produce sebum. In other words, the medication stops androgens from being able to stimulate these glands to produce more skin oil. In theory, this should prevent the overproduction of skin oil.9 However, since clascoterone is a very new medication, exactly how it helps with acne is still being studied and is not fully understood.
So far, clinical trials have shown that clascoterone can produce modest results, reducing facial acne by about 20% in both males and females. In the longest-running trial, patients applied clascoterone to the skin daily for 9 months, and there were no serious or so-called systemic (whole body) side effects.10,11 However, this topical hormonal treatment has only been on the market for a short time, so we will need to see more data on how safe and effective it is over the longer term.
Expand to read details of studies

A study published in the journal JAMA Dermatology in 2020 investigated the safety and efficacy of 1% clascoterone cream for the treatment of acne. A total of 1440 patients, both males and females, applied clascosterone cream to their faces twice a day for 12 weeks. At the end of the treatment period, the patients had approximately 20% fewer acne lesions on average compared to before the treatment. The most common side effect was mild skin redness.10

An article published in the journal Clinical, Cosmetic and Investigational Dermatology in 2022 reviewed the evidence available to date from clinical trials on clascoterone. The article authors concluded that both males and females with acne can achieve a noticeable reduction in acne by using topical clascoterone cream, and that side effects are rare and tend to be mild. The authors wrote, “Not only do clinical trials show efficacy for reduction in total acne lesion counts, it has a significantly tolerable safety profile even at nine months of treatment.”11
Facial Hair – It’s Important to Shave Every Day If Applying Topical Medications
Males develop facial hair and facial hair can make it harder to apply topical acne medications. Even just a bit of stubble can make it difficult to apply medication evenly across the skin. The longer facial hair becomes, the more it grabs on to topical treatments and prevents those treatments from penetrating into the skin where they are needed. For this reason, it is best for males who are regularly applying topical acne treatments to shave every day.
Another important reason to shave every day is to prevent irritation. The longer facial hair becomes, the more difficult it is to shave, which can lead to more irritation when shaving. Since irritation aggravates acne, this is another reason for males who are using topical treatments to shave every day.
Some Acne Treatments May Work Better in Females
Doctors can prescribe non-hormonal treatments to males and females without any risk of feminizing males. However, even non-hormonal treatments appear to sometimes work differently in males compared with females.
For instance, 2 studies that treated acne with a combination clindamycin phosphate/benzoyl peroxide gel found that this medication may be more effective in females.12,13
Expand to read details of studies

A 2015 study in the Journal of Drugs in Dermatology found that the “change from baseline in inflammatory and noninflammatory lesion counts was greater among females than males,” and that the clindamycin phosphate/benzoyl peroxide “appears to be more effective in female patients.”12

A 2012 study involving adolescent patients, also in the Journal of Drugs in Dermatology, found that the same clindamycin phosphate/benzoyl peroxide gel was more effective in females than in males, but that the difference was small and only slightly significant.13
Another study looked at a topical anti-inflammatory acne medication called dapsone and found that it too worked better in females.14
Expand to read details of study

Another 2012 study in the Journal of Drugs in Dermatology, in which patients were treated with dapsone gel for 12 weeks, found that females responded better to the dapsone than males.
Females:
- Had a greater reduction in various types of acne lesions.
- Had a higher clinical success rate.14
Yet another study looked at the efficacy of a topical retinoid, tretinoin, for the treatment of moderate-to-severe acne and found that it works a little better in females.15
Expand to read details of study

A 2019 study, again in the Journal of Drugs in Dermatology, compared the efficacy of 0.05% tretinoin lotion in females versus males with moderate-to-severe acne. After 12 weeks of treatment, females experienced a 51.7% reduction in acne lesions, compared to 46.1% in males. The researchers concluded that tretinoin lotion might be somewhat more effective for females with moderate-to-severe acne than for males.15
A final study looked at the oral medication isotretinoin and showed no difference in efficacy between males and females.16
Expand to read details of study
A 2014 study in the Journal of Clinical & Experimental Dermatology Research, in which patients were treated with isotretinoin, a medication that is typically reserved for the most severe forms of acne, found no differences between male and female response to treatment. However, the authors noted that the females in this study had other conditions such as polycystic ovary syndrome, as well as less severe acne at the beginning of the study, which might have affected the study results.16
Recent Research Shows Males and Females Are Equally Careful about Sticking to Their Treatment Plan
While some older studies found that males were less likely to stick to their treatment plan compared to females, recent research suggests this may not be the case.17,18 For example, a study published in the Journal of International Medical Research in 2019 looked at a total of 250 patients and found that both males and females were equally likely to carefully follow their acne treatment plan.18 In other words, if certain acne medications work better for females, it may not be because females are simply better at following their doctor’s orders.
Conclusion
The make-up of male and female skin differs, and each type responds differently to treatment. Hormonal treatments are far more commonly used for females than for males, and some non-hormonal treatments seem to work slightly better on females when compared to male skin. The exception being isotretinoin, which may treat both skin types equally.
References
- Dao, H., Jr. & Kazin, R. A. Gender differences in skin: a review of the literature. Gend. Med. 4, 308 – 328 (2007). https://www.ncbi.nlm.nih.gov/pubmed/18215723
- Kim, M. K. et al. Evaluation of gender difference in skin type and pH. J. Dermatol. Sci. 41, 153 – 156 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16406502
- Zouboulis, C. C. et al. What is the pathogenesis of acne? Exp. Dermatol. 14, 143 – 152 (2005). https://www.ncbi.nlm.nih.gov/pubmed/15679586
- Zouboulis, C. C., Chen, W. C., Thornton, M. J., Qin, K. & Rosenfield, R. Sexual hormones in human skin. Horm. Metab. Res. 39, 85 – 95 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17326004
- Thiboutot, D., Gilliland, K., Light, J. & Lookingbill, D. Androgen metabolism in sebaceous glands from subjects with and without acne. Arch. Dermatol. 135, 1041 – 1045 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10490108
- Wiegratz, I. & Kuhl, H. Managing cutaneous manifestations of hyperandrogenic disorders: the role of oral contraceptives. Treat. Endocrinol. 1, 372 – 386 (2002). https://www.ncbi.nlm.nih.gov/pubmed/15832490
- Sweeney, T. M., Szarnicki, R. J., Strauss, J. S. & Pochi, P. E. The effect of estrogen and androgen on the sebaceous gland turnover time. J. Invest. Dermatol. 53, 8 – 10 (1969). https://www.ncbi.nlm.nih.gov/pubmed/5793140
- Marynick, S. P., Chakmakjian, Z. H., McCaffree, D. L. & Herndon, J. H., Jr. Androgen excess in cystic acne. N. Engl. J. Med. 308, 981 – 986 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6220224
- Kalabalik-Hoganson, J., Frey, K. M., Ozdener-Poyraz, A. E. & Slugocki, M. Clascoterone: A novel topical androgen receptor inhibitor for the treatment of acne. Ann. Pharmacother. 55, 1290-1296 (2021). https://pubmed.ncbi.nlm.nih.gov/33533262/
- Hebert, A., Thiboutot, D., Stein Gold, L., Cartwright, M., Gerloni, M., Fragasso, E. & Mazzetti, A. Efficacy and safety of topical clascoterone cream, 1%, for treatment in patients with facial acne: Two Phase 3 randomized clinical trials. JAMA Dermatol. 156, 621-630 (2020). https://pubmed.ncbi.nlm.nih.gov/32320027/
- Sanchez, C. & Keri, J. Androgen receptor inhibitors in the treatment of acne vulgaris: Efficacy and safety profiles of clascoterone 1% cream. Clin. Cosmet. Investig. Dermatol. 15, 1357-1366 (2022). https://pubmed.ncbi.nlm.nih.gov/35874458/
- Harper, J. C. The efficacy and tolerability of a fixed combination clindamycin (1.2%) and benzoyl peroxide (3.75%) aqueous gel in patients with facial acne vulgaris: gender as a clinically relevant outcome variable. J. Drugs Dermatol. 14, 381 – 384 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25844612
- Harper, J. C. Gender as a clinically relevant outcome variable in acne: benefits of a fixed combination clindamycin phosphate (1.2%) and benzoyl peroxide (2.5%) aqueous gel. J. Drugs Dermatol. 11, 1440 – 1445 (2012). https://www.ncbi.nlm.nih.gov/pubmed/23377514
- Tanghetti, E., Harper, J. C. & Oefelein, M. G. The efficacy and tolerability of dapsone 5% gel in female vs male patients with facial acne vulgaris: gender as a clinically relevant outcome variable. J. Drugs Dermatol. 11, 1417 – 1421 (2012). https://www.ncbi.nlm.nih.gov/pubmed/23377510
- Lain, E., Day, D., Harper, J. & Guenin, E. Tretinoin 0.05% lotion for the once-daily treatment of moderate-to-severe acne vulgaris: Impact of gender and race on efficacy and safety. J. Drugs Dermatol. 18, 1128-1138 (2019). https://pubmed.ncbi.nlm.nih.gov/31741356/
- Pampena NS, et al. Gender matter in isotretinoin therapy for acne vulgaris? A retrospective study. J. Clin. Exp. Dermatol. Res. 6, 3 – 7 (2015). https://www.longdom.org/open-access/gender-matter-in-isotretinoin-therapy-for-acne-vulgaris-a-retrospective-study-2155-9554-10000300.pdf
- Keaney, T. C. Male acne: the importance of gender in acne treatment. Cutis. 91, 167 – 168 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23763071
- Sevimli Dikicier, B. Topical treatment of acne vulgaris: efficiency, side effects, and adherence rate. J. Int. Med. Res. 47, 2987 – 2992 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31122106
 Acne.org Products
Acne.org Products